Oral Hygiene &Treatment of Gum Disease
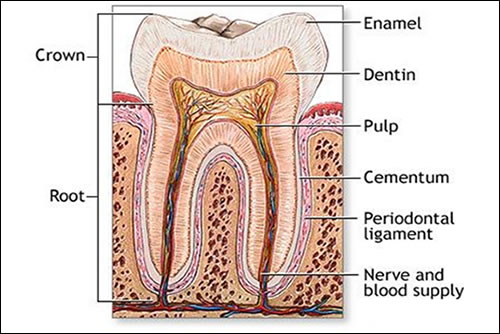
Tooth anatomy
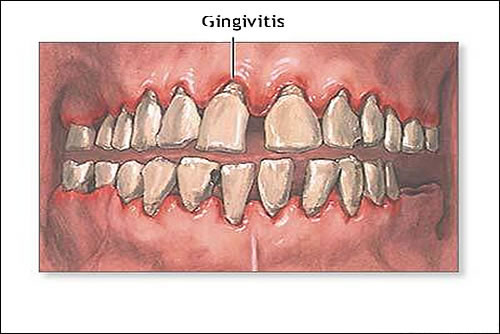
The structure of the tooth includes dentin, pulp and other tissues, blood vessels and nerves imbedded in the bony jaw. Above the gum line, the tooth is protected by the hard enamel covering. Gingivitis is inflammation of the gums (gingiva).
Causes, incidence, and risk factors
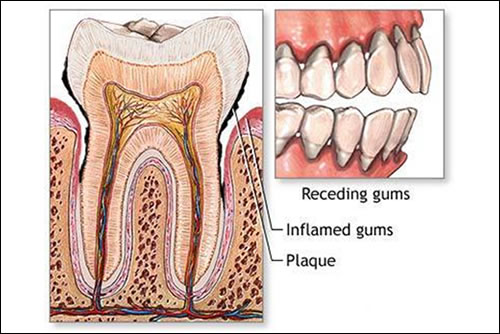
Gingivitis is a form of periodontal disease. Periodontal disease involves inflammation and infection that destroys the tissues that support the teeth, including the gums, the periodontal ligaments, and the tooth sockets (alveolar bone).
Gingivitis is due to the long-term effects of plaque deposits. Plaque is a sticky material made of bacteria, mucus, and food debris that develops on the exposed parts of the teeth. It is a major cause of tooth decay. If you do not remove plaque, it turns into a hard deposit called tartar that becomes trapped at the base of the tooth. Plaque and tartar irritate and inflame the gums. Bacteria and the toxins they produce cause the gums to become infected, swollen, and tender.
Injury to the gums from any cause, including overly vigorous brushing or flossing of the teeth, can cause gingivitis.
The following raise your risk for developing gingivitis:
- General illness
- Poor dental hygiene
- Pregnancy (hormonal changes increase the sensitivity of the gums)
- Uncontrolled diabetes
Misaligned teeth, rough edges of fillings, and ill-fitting or unclean mouth appliances (such as braces, dentures, bridges, and crowns) can irritate the gums and increase the risk of gingivitis. Medications such as phenytoin and birth control pills, and heavy metals such as lead and bismuth are also associated with gingivitis.
Many people have gingivitis to a varying degree. It usually develops during puberty or early adulthood due to hormonal changes and may persist or recur frequently, depending on the health of your teeth and gums.
Symptoms
• Bleeding gums (blood on toothbrush even with gentle brushing of the teeth)
• Bright red or red-purple appearance to gums
• Gums that are tender when touched, but otherwise painless
• Mouth sores
• Swollen gums
• Shiny appearance to gums
Signs and tests
The dentist will examine your mouth and teeth and look for soft, swollen, red-purple gums. Deposits of plaque and tartar may be seen at the base of the teeth. The gums are usually painless or mildly tender.
No further testing is usually necessary, although dental x-rays and dental bone measurements may be done to determine whether the inflammation has spread to the supporting structures of the teeth.
See: Periodontitis
Treatment
The goal is to reduce inflammation. The teeth are cleaned thoroughly by the dentist or dental hygienist. This may involve various instruments or devices to loosen and remove deposits from the teeth.
Careful oral hygiene is necessary after professional tooth cleaning. The dentist or hygienist will show you how to brush and floss. Professional tooth cleaning in addition to brushing and flossing may be recommended twice per year or more frequently for severe cases.
Antibacterial mouth rinses or other aids may be recommended in addition to frequent, careful, tooth brushing and flossing.
Repair of misaligned teeth or replacement of dental and orthodontic appliances may be recommended. Any other related illnesses or conditions should be treated.
Expectations (prognosis)
The removal of plaque from inflamed gums may be uncomfortable. Bleeding and tenderness of the gums should lessen within 1 or 2 weeks after professional cleaning and careful oral hygiene. Warm salt water or antibacterial rinses can reduce the puffiness. Over-the-counter anti-inflammatory medications will ease any discomfort from a rigorous cleaning.
Healthy gums are pink and firm in appearance. Strict oral hygiene must be maintained for your whole life or gingivitis will recur.
Complications
• Recurrence of gingivitis
• Periodontitis
• Infection or abscess of the gingiva or the jaw bones
• Trench mouth
Calling your health care provider
Call your dentist if symptoms of gingivitis are present, especially if you have not had a routine cleaning and examination in the last 6 months.
Call your health care provider if the dentist recommends medical treatment of underlying conditions that contribute to the development of gingivitis.
Prevention
Good oral hygiene is the best prevention against gingivitis because it removes the plaque that causes the disorder. The teeth should be brushed at least twice daily and flossed gently at least once per day. For people who are prone to gingivitis, brushing and flossing may be recommended after every meal and at bedtime. Consult the dentist or dental hygienist for instructions on proper brushing and flossing techniques.
Special appliances or tools may be recommended by the dentist for use by people who are particularly prone to plaque deposits. The use of supplements does not replace thorough brushing and flossing. Appliances and tools may include special toothpicks, toothbrushes, water irrigation, or other devices.
Antiplaque or antitartar toothpastes or mouth rinses may be recommended by the dentist or dental hygienist.
Regular professional tooth cleaning is important to remove plaque that may develop even with careful brushing and flossing. Many dentists recommend having the teeth professionally cleaned at least every 6 months.
Gingivitis
Inflammation of the gums is called gingivitis. Bacteria in plaque around the teeth release enzymes (collagenases) that can damage and erode the gum tissues.
The infected gums swell, bleed easily, recede, and loosen from the teeth. Tooth loss is caused more frequently by gum disease than tooth decay.